
Resources
Our Publications
Research and insights from our team at EpiDriver. Our publications include scientific articles, reports, and educational materials.
External Publications
Highlights from key studies, articles, and resources that inspire and complement EpiDriver’s mission.
RESEARCH FRAMEWORKS IN HEALTHCARE
Our topics are related to public health, healthcare access, behavior change, and environmental health indicators.
These topics are relevant for understanding and addressing health inequalities, infectious diseases, non-communicable diseases, and health promotion. We emphasizes the importance of people-centered care and decision-making processes in healthcare.
Our content provides valuable insights into the complex interactions between people, their environments, and health outcomes. Furthermore, it can further elaborate on these theories or models for a more comprehensive understanding.
Ecosocial Theory:
is a broad and complex theory with the purpose of describing and explaining causal relationships in disease distribution. While it incorporates biological and psychosocial influences on disease occurrence, the theory is also suited to analyze the relationships between social factors and disease development in public health research. The core constructs of Ecosocial Theory are: Embodiment; Pathways to Embodiment; the cumulative interplay between exposure, resistance, and susceptibility; and agency and accountability. Further, the theory specifies that all constructs must be considered in concert, as they work together in a synergistic explanation of disease distribution. The theory assumes that distributions of disease are determined at multiple levels and that analyses must incorporate historical, political economic, temporal, and spatial analyses.
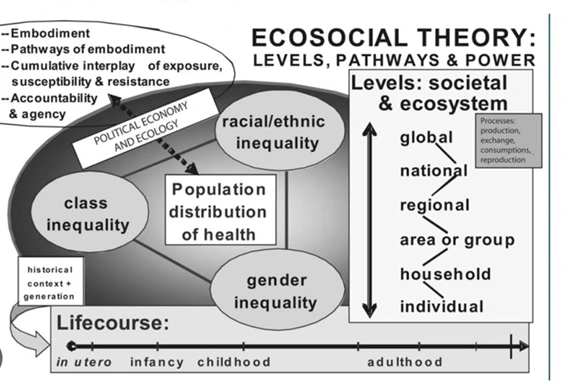
(This graphic is adapted to the colors and designs of the brand)
Nancy Krieger, Theories for social epidemiology in the 21st century: an ecosocial perspective, International Journal of Epidemiology, Volume 30, Issue 4, August 2001, Pages 668–677, https://doi.org/10.1093/ije/30.4.668
What related topic projects is it suitable for?
- Epidemiological surveillance
- Disease development
- Health inequalities
- Healthcare access
Ecological model:
“…the interaction between, and interdependence of, factors within and across all levels of a health problem. It highlights people’s interactions with their physical and sociocultural environments.”
Ecological models recognize multiple levels of influence on health behaviors, including:
- Intrapersonal/individual factors, which influence behavior such as knowledge, attitudes, beliefs, and personality.
- Interpersonal factors, such as interactions with other people, which can provide social support or create barriers to interpersonal growth that promotes healthy behavior.
- Institutional and organizational factors, including the rules, regulations, policies, and informal structures that constrain or promote healthy behaviors.
- Community factors, such as formal or informal social norms that exist among individuals, groups, or organizations, can limit or enhance healthy behaviors.
- Public policy factors, including local, state, and federal policies and laws that regulate or support health actions and practices for disease prevention including early detection, control, and management.
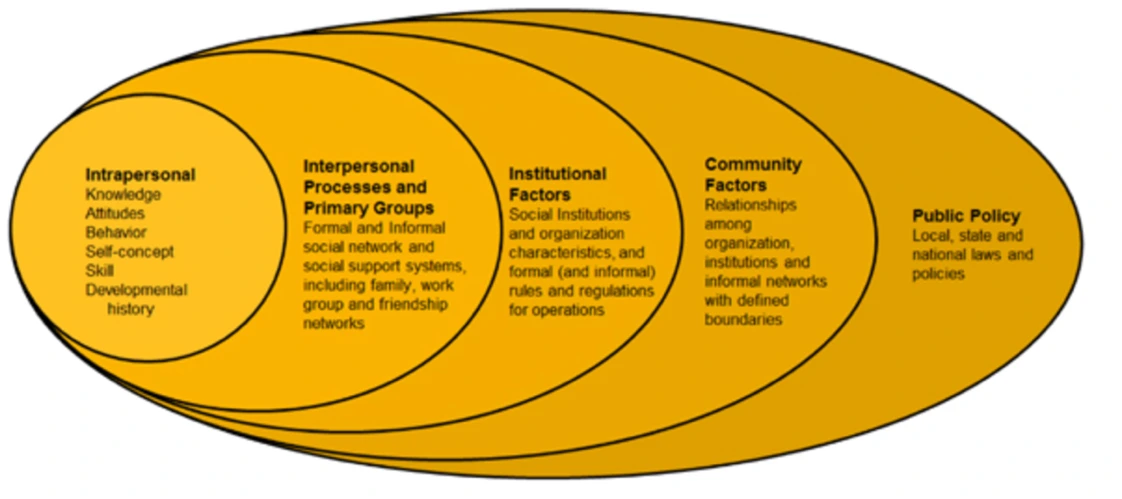
(This graphic is adapted to the colors and designs of the brand)
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988 Winter;15(4):351-77.
What related topic projects is it suitable for?
- Health behaviors
- Making decision process in health
- Health inequalities
- Healthcare access
The health belief model:
The Health Belief Model predicts that a specific health behavior is more or less likely based on an individual’s perceptions of disease severity and personal susceptibility to the disease combined with perceived benefits and barriers to that behavior. For an individual to adopt a specific behavior, the perception of the threat of disease and the benefits of the health behavior must outweigh the perceived barriers. Personal factors, sense of self-efficacy, and cues to action are also frequently included in the model. The Health Belief Model is most applicable to behavior change interventions for patients.
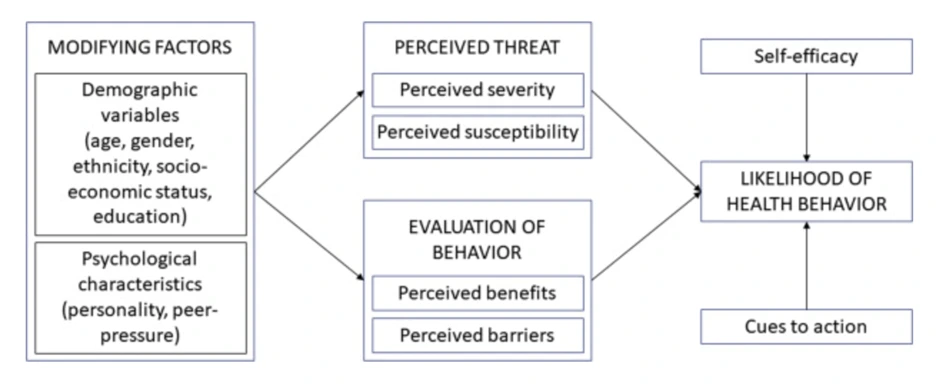
(This graphic is adapted to the colors and designs of the brand)
Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–183.
What related topic projects is it suitable for?
- Health behaviors
- Self efficacy
- Healthcare interventions
- Treatment adherence
Transtheoretical model:
The TTM posits that individuals move through six stages of change: precontemplation, contemplation, preparation, action, maintenance, and termination. Termination was not part of the original model and is less often used in application of stages of change for health-related behaviors. For each stage of change, different intervention strategies are most effective at moving the person to the next stage of change and subsequently through the model to maintenance, the ideal stage of behavior.
- Precontemplation – In this stage, people do not intend to take action in the foreseeable future (defined as within the next 6 months). People are often unaware that their behavior is problematic or produces negative consequences. People in this stage often underestimate the pros of changing behavior and place too much emphasis on the cons of changing behavior.
- Contemplation – In this stage, people are intending to start the healthy behavior in the foreseeable future (defined as within the next 6 months). People recognize that their behavior may be problematic, and a more thoughtful and practical consideration of the pros and cons of changing the behavior takes place, with equal emphasis placed on both. Even with this recognition, people may still feel ambivalent toward changing their behavior.
- Preparation (Determination) – In this stage, people are ready to take action within the next 30 days. People start to take small steps toward the behavior change, and they believe changing their behavior can lead to a healthier life.
- Action – In this stage, people have recently changed their behavior (defined as within the last 6 months) and intend to keep moving forward with that behavior change. People may exhibit this by modifying their problem behavior or acquiring new healthy behaviors.
- Maintenance – In this stage, people have sustained their behavior change for a while (defined as more than 6 months) and intend to maintain the behavior change going forward. People in this stage work to prevent relapse to earlier stages.
- Termination – In this stage, people have no desire to return to their unhealthy behaviors and are sure they will not relapse. Since this is rarely reached, and people tend to stay in the maintenance stage, this stage is often not considered in health promotion programs.
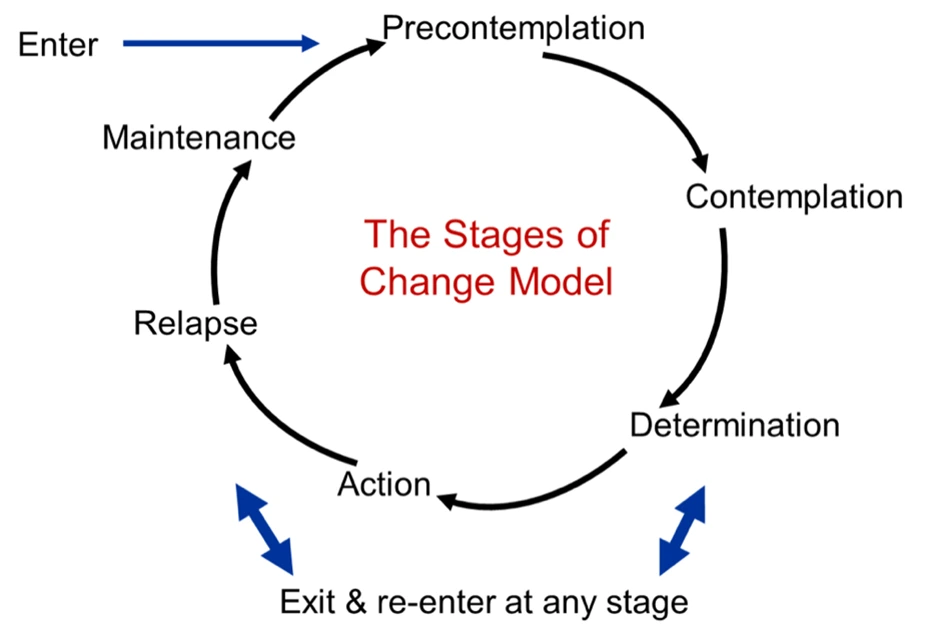
(This graphic is adapted to the colors and designs of the brand)
Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997 Sep-Oct;12(1):38-48. doi: 10.4278/0890-1171-12.1.38.
What related topic projects is it suitable for?
- Treatment adherence
- Health behaviors
- Healthcare interventions
- Change process
Social cognitive theory:
(SCT) describes the influence of individual experiences, the actions of others, and environmental factors on individual health behaviors. SCT provides opportunities for social support through instilling expectations, self-efficacy, and using observational learning and other reinforcements to achieve behavior change.
Key components of the SCT related to individual behavior change include:
- Self-efficacy: The belief that an individual has control over and is able to execute a behavior.
- Behavioral capability: Understanding and having the skill to perform a behavior.
- Expectations: Determining the outcomes of behavior change.
- Expectancies: Assigning a value to the outcomes of behavior change.
- Self-control: Regulating and monitoring individual behavior.
- Observational learning: Watching and observing outcomes of others performing or modeling the desired behavior.
- Reinforcements: Promoting incentives and rewards that encourage behavior change.
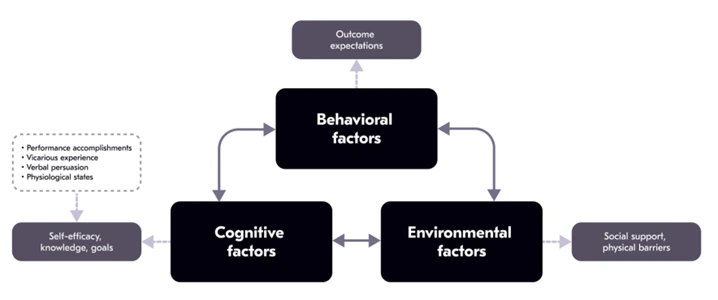
(This graphic is adapted to the colors and designs of the brand)
Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1-26. doi: 10.1146/annurev.psych.52.1.1.
What related topic projects is it suitable for?
- Treatment adherence
- Health behaviors
- Healthcare interventions
- Change process
Integrated health risk model:
The idea behind is that an integrated approach to risk management and population health can combines the “key elements of both fields can provide a more comprehensive and more powerful approach to addressing critical health issues” (Krewski et al., 2007). Among the key population, “health elements are the prominence of the determinants of health and the inclusion of a wide range of risk management interventions, including interventions based on community action” (Krewski et al., 2007). In this sense, “health risk science corresponds to the risk assessment component of the traditional risk frameworks, with health risk policy analysis reflecting the risk management component” (Krewski et al., 2007). As can be seen, the integrated framework is built on three categories of health determinants: “biological and genetic determinants (such as genetic endowment, the functioning of various body systems, and the processes of development and aging); environmental and occupational determinants (including the physical environment, both natural and human-built, and employment and working conditions); and social and behavioral determinants (such as income and social status, social support networks, education, personal health practices and coping skill, gendered norms, and culture) and their interactions” (Krewski et al., 2007).
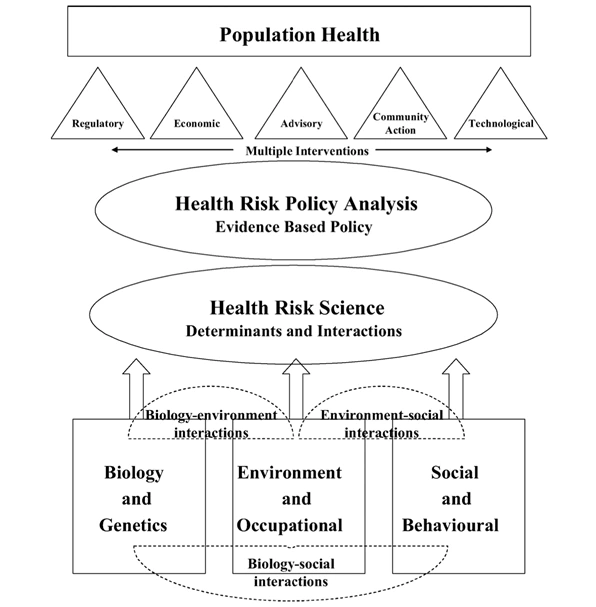
(This graphic is adapted to the colors and designs of the brand)
Krewski, D., Hogan, V., Turner, M. C., Zeman, P. L., McDowell, I., Edwards, N. & Losos, J. (2007). An Integrated Framework for Risk Management and Population Health. Human and Ecological Risk Assessment: An International Journal, 13(6), 1288–1312.
What related topic projects is it suitable for?
- Health inequalities
- Healthcare access
- Health disease process
- infectious diseases
- Non communicable diseases
DPSEEA framework:
An alternative to the DPSIR Framework is the Driving force-Pressure-State-Exposure-Effect-Action (DPSEEA) Framework. DPSEEA has been widely used in European and international health assessments (Corvalan et al., 1999).
- In the DPSEEA conceptual framework, Drivers are the social, demographic and economic developments in societies and the corresponding changes in life styles, overall levels of consumption and production patterns.
- Drivers function through human activities which may intentionally or unintentionally exert Pressures on the environment.
- The pressures exerted by society may lead to unintentional or intentional changes in the State of the environment.
- Factors such as human behavioral and lifestyle choice will influence individual Exposure to environmental challenges.
- Humans take Action by making decisions to reduce the Effects on human health.
However, by emphasizing the link between environmental degradation and human health, DPSEEA de-emphasized elements of the DPSIR framework, such as natural capital provided by ecosystems (Impact) that is a core concept of sustainability.
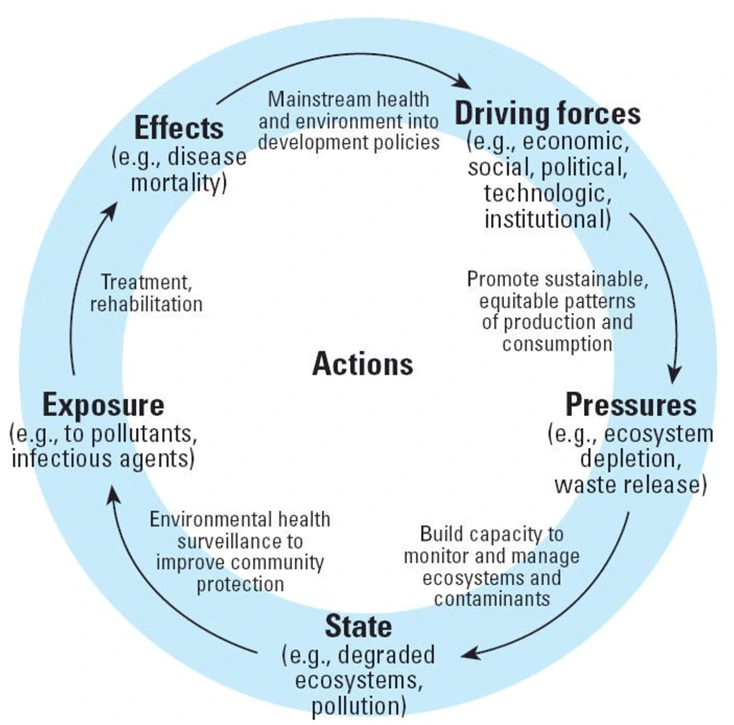
(This graphic is adapted to the colors and designs of the brand)
Carneiro FF, Oliveira ML, Netto GF, Galvão LA, Cancio JA, Bonini EM, Corvalan CF. Meeting report: development of environmental health indicators in Brazil and other countries in the americas. Environ Health Perspect. 2006 Sep;114(9):1407-8.
What related topic projects is it suitable for?
- Change process
- Air pollution
- Disease mortality
- Infectious diseases
- Climate change
The Health Equity Framework:
ETR’s Health Equity Framework is a model that describes the ways that health and education outcomes are influenced by complex interactions between people and their environments.
The Health Equity Framework is ETR’s shared language for talking about health and education equity. The Framework is also a reflection tool to assess approaches to health equity and explore new pathways for learning.
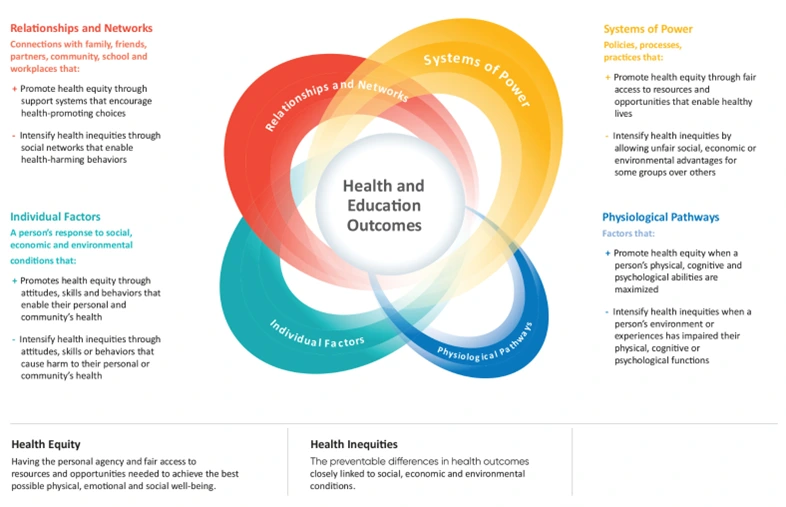
Peterson A, Charles V, Yeung D, Coyle K. The Health Equity Framework: A Science- and Justice-Based Model for Public Health Researchers and Practitioners. Health Promotion Practice. 2021;22(6):741-746.
What related topic projects is it suitable for?
- Disparities analysis
- Health inequalities
- Healthcare access
- Health disease process
- infectious diseases
- Non communicable diseases
Primary Healthcare:
Primary care is a model of care that supports first-contact, accessible, continuous, comprehensive and coordinated person-focused care. It aims to optimize population health and reduce disparities across the population by ensuring that subgroups have equal access to services. There are five core functions of primary care:

- First contact accessibility creates a strategic entry point for and improves access to health services.
- Continuity promotes the development of long-term personal relationships between a person and a health professional or a team of providers.
- Comprehensiveness ensures that a diverse range of promotive, protective, preventive, curative, rehabilitative, and palliative services are provided.
- Coordination organizes services and care across levels of the health system and over time.
- People-centred care ensures that people have the education and support needed to make decisions and participate in their own care.
Macinko J, Montenegro H, Nebot Adell C, Etienne C; Grupo de Trabajo de Atención Primaria de Salud de la Organización Panamericana de la Salud. La renovación de la atención primaria de salud en las Américas [Renewing primary health care in the Americas]. Rev Panam Salud Publica. 2007 Feb-Mar;21(2-3):73-84. Spanish.
What related topic projects is it suitable for?
- Healthcare access
- Disparities reduction
- Healthcare provision
- Health promotion
Theory of reasoned action and theory of planned behavior
Two closely associated theories — The Theory of Reasoned Action and the Theory of Planned Behavior — suggest that a person’s health behavior is determined by their intention to perform a behavior. A person’s intention to perform a behavior (behavioral intention) is predicted by 1) a person’s attitude toward the behavior, and 2) subjective norms regarding the behavior. Subjective norms are the result of social and environmental surroundings and a person’s perceived control over the behavior. Generally, positive attitude and positive subjective norms result in greater perceived control and increase the likelihood of intentions governing changes in behavior.
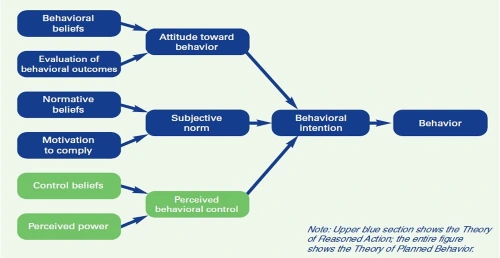
(This graphic is adapted to the colors and designs of the brand)
Source: Hackman CL, Knowlden AP. Theory of reasoned action and theory of planned behavior-based dietary interventions in adolescents and young adults: a systematic review. Adolesc Health Med Ther. 2014 Jun 6;5:101-14.
What related topic projects is it suitable for?
- Health promotion
- Health behaviors
- Change process
EpiDriver ©2025 / All rights reserved.